Otorrhoea
Flowchart
Red flags requiring urgent ENT referral
Associated facial nerve palsy
Spreading cellulitis
Suspected mastoiditis (red, tender lump behind ear in unwell patient with AOM)
Systemically unwell
Neurological signs
Assessment and recognition
History
How long has your ear been discharging? Does it come and go?
Colour of discharge? Offensive smell?
Other otological symptoms (pain, tinnitus, hearing loss, vertigo, facial weakness)
Water exposure? Cotton buds?
Any previous ear problems or operations?
PMH (especially diabetes or other immunocompromising conditions)
Smoking status
Examination
Inspect the ear, looking for discharge/crust, cellulitis, post-aural bulge and redness, scars.
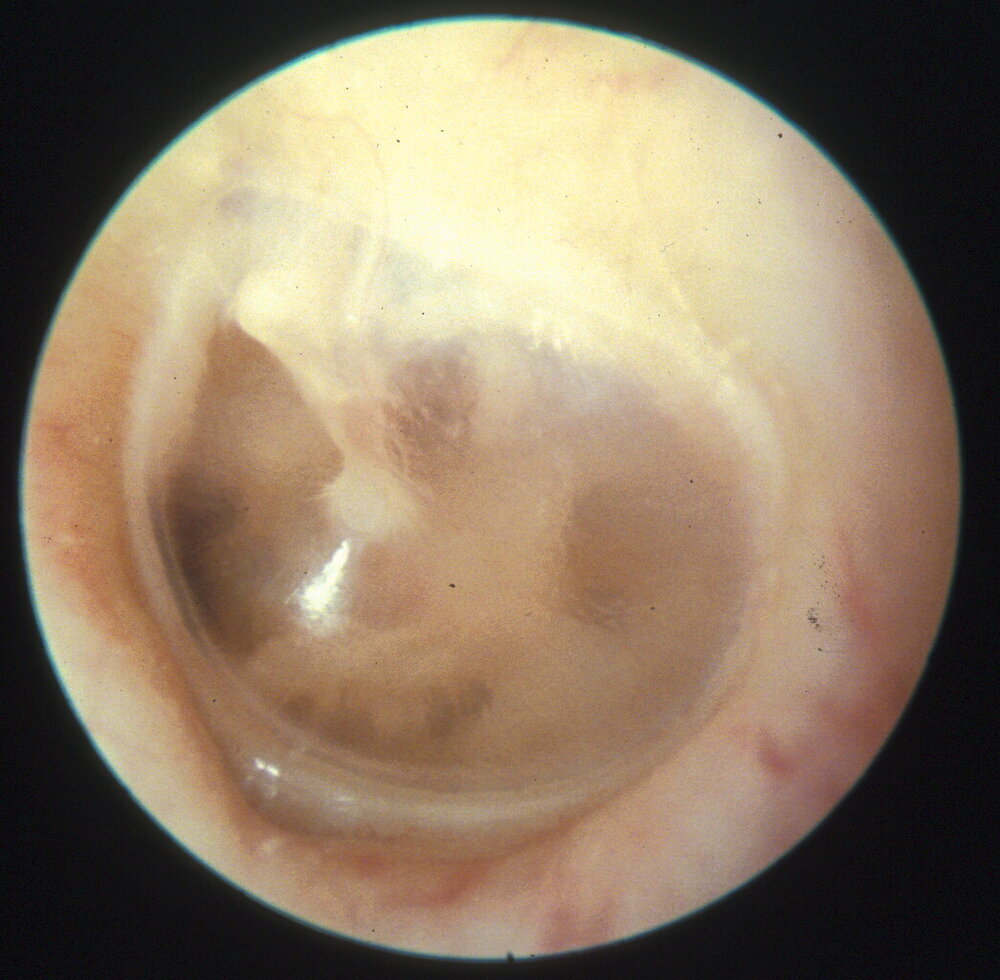
Otoscopy - look for otitis externa, perforation +/- purulent/pulsatile discharge, ear drum retraction with debris or crust (ensure you check up in the attic)
Facial nerve exam
Normal Tympanic
Membrane
Left or right side?
Differential diagnosis and primary care management
Acute conditions
Otitis externa - inflammation of the ear canal lining. Examination would reveal a red, oedematous ear canal with thick, coated exudate. The tympanic membrane may not be visible but should be normal. Give a two-week course of antibiotic-steroid eardrops (e.g. Gentisone HC or Sofradex) and water precautions. No need to swab initially. If not settling, refer to ENT emergency clinic.
Otitis Externa
For more info, please click here
Acute otitis media - This is inflammation of the middle ear mucosa and normally presents in children. There is usually an onset of pain before the exudate appears. Examination at initial stages would reveal a bulging and red TM, which can perforate to allow the pus to discharge into the external ear. This usually results in the pain and fever resolving. Follow NICE guidance and prescribe antibiotics if patient remains unwell after an initial trial of analgesia. Some patients develop more prolonged painless discharge after AOM via the perforation - give two week of ciprofloxacin drop to prevent this becoming chronic.
For more info, please click here
Acute Otitis Media
Left or right side?
CSF otorrhoea - Rare. CSF is perfectly clear and watery. Usually occurs after head trauma or occasionally skull base/ear surgery. The diagnosis is confirmed by testing for tau protein/beta-trace. Many cases settle spontaneously; antibiotic coverage is not required. Refer urgently to Otology/ENT.
For more info, please click here
Chronic
Chronic otitis media - should be suspected in all patients with a chronically/intermittently discharging ear. The discharge is often malodorous. Perform otoscopy looking for a perforation (with or without active discharge), or a retraction pocket with keratin/debris in it. Patients should be referred routinely to Otology/ENT, unless there are red flags.
For more info, please click here
Referral pathways
Same day
Complications of acute otitis media
Complications of acute otitis externa
Button battery in ear canal
Temporal bone fracture (assessment by ED)
Cancer pathway
Unexplained growth in ear canal which bleeds on contact
ENT emergency clinic
Non-resolving acute otitis externa (trial two weeks of Sofradex/Cilodex/Gentisone
Foreign bodies in ear canal
Routine
Chronic otitis media
Author: Mr Ananth Vijendren BM MRCS MRCS (ENT) FRCS (ORL-HNS) PhD, Consultant Otologist/ENT Surgeon, Lister Hospital, Stevenage