Nasal Blockage
Flowchart
Red flags
Unilateral nasal obstruction associated with serosanguinous nasal discharge and/or pain may rarely be due to sinonasal malignancy. This is an indication for cancer-wait pathway referral.
Common pitfalls
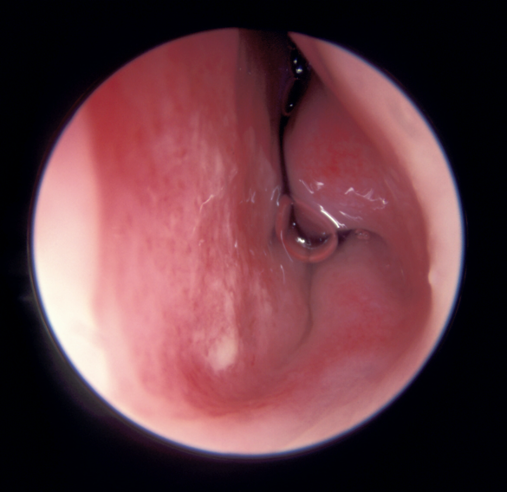
Nasal polyps are not commonly visible on anterior rhinoscopy. More often, you are seeing a hypertrophic inferior turbinate. The inferior turbinate arises from the lateral nasal wall and is pink-red.
Regular, long-term use of an intranasal steroid spray is the mainstay of managing almost all nasal inflammatory disease. Patients must be made aware that these are long-term daily medications, and not to expect results before 6-8 weeks of use. Systemic absorption of intranasal fluticasone and mometasone is negligible - continue long-term if nasal blockage is improved.
Sinus tenderness is of no clinical value in diagnosis.
History
How long has your nose felt blocked?
Is it one or both sides? Or does it alternate?
Do you get lots of nasal discharge? Clear or coloured? (coloured rhinorrhoea suggests CRS)
Do you have a reduced sense of smell? (suggests CRS)
Do you have an unpleasant smell in your nose? (suggests CRS without polyps)
Do you have sneezing, itching or itchy, watery eyes? (suggests allergy)
Any facial pain?
Are your symptoms worse at any time of the year or time of the day?
Have you had any operations on your nose in the past?
Have you had any injuries to your nose in the past?
What treatments have you tried so far?
Occupation
Smoking or cocaine use
Inspection
Patients with allergic disease can occasionally have classical signs such as dark circles and an “allergic crease” across the nose.
Examine for lateral deviation of the nose, indicating septonasal deformity which may contribute to blockage.
Internal examination
Complete examination of the nose in rhinorrhoea requires an endoscope.
However, using an otoscope, or a headlight and a Thudichum speculum, look for:
Septal deviation
Hypertrophic, oedematous mucosa suggestive of rhinitis (or CRS)
Septal perforation and/or crusting
Mucopurulent secretions
Normal nasal cavity
and a septal spur
Which nostril is this?
o Boggy, moist nasal mucosa and oedematous inferior turbinates typical of rhinitis:
Rhinitis
o Occasionally, mucopus or polyposis may be visible, indicating chronic rhinosinusitis (usually these are not visible without an endoscope):
Nasal Polyp
Differential diagnosis:
Chronic rhinosinusitis (CRS) +/- nasal polyps
Syndrome of chronic inflammation of the nose and paranasal sinuses. The four key symptoms of CRS are nasal obstruction, rhinorrhoea, reduced smell and facial pain.
First line treatment is regular nasal fluticasone or mometasone spray (for at least 3 months), plus regular saline irrigation. If effective, continue long term. Consider a short course of prednisolone +/- antibiotics at start of treatment if symptoms are severe.
If first-line treatment is not effective, refer routinely to ENT/rhinology.
Rhinitis
Chronic nasal cavity inflammation: either allergic or non-allergic (idiopathic, autonomic, hormonal etc). Patients usually have rhinorrhoea with bilateral/alternating nasal congestion, but may have rhinorrhoea alone. Allergic rhinitis is more strongly associated with clear rhinorrhoea, sneezing, itching or an atopic background.
In mild allergic-type symptoms without significant nasal blockage, consider a second-generation antihistamine with or without nasal saline irrigation.
In moderate symptoms (especially if congested), start fluticasone/mometasone nasal spray for at least a 3-month trial. Consider also giving oral AH if prominent sneezing/itching.
Dymista nasal spray (fluticasone + azelastine) is second-line for allergic rhinitis, if patients do not respond to first-line steroid sprays.
Rhinitis medicamentosa
Rebound nasal congestion caused by overuse of a nasal decongestant (>2 weeks). Management is to stop the decongestant, supported by regular use of a nasal steroid spray.
Septal or septonasal deviation
This usually causes unilateral, persistent blockage. It can present as a long-term stable blockage, or after an injury. Be aware than many patients have incidental minor deviations, and blockage that is in fact caused by inflammatory disease. These patients will have bilateral or alternating blockage.
Significant septal deviation is usually (but not always) visible on anterior rhinoscopy. If there is bilateral congestion or evidence of inflammation, please give a three-month trial of intranasal steroid spray before deciding on referral.
Moderate septal deviation is treated with septoplasty. Severe complex septal deviation (especially when associated with external deformity) is treated with septorhinoplasty.
Tumours
Benign tumours include classical papillomas, inverted papillomas, and other rarer masses.
Malignant sinonasal tumours are rare, and have many types include squamous cell carcinoma, lymphoma, melanoma and adenocarcinoma. They present with unilateral nasal symptoms including obstruction, epistaxis, and in more advanced cases orbital and intracranial manifestations.
A mass involving the postnasal space can cause unilateral glue ear (OME), which is a red flag in adults. These patients must be referred via the cancer-wait pathway to ENT.
Management in primary care/when to refer
Refer any patient with unilateral blockage and serosanguinous discharge or other red-flag symptoms via the cancer wait pathway.
Patients with a persistent, unilateral nasal blockage and a significant septal and/or nasal deviation to the same side can be referred routinely for consideration of surgical treatment. Note that septorhinoplasty is not usually funded for external deformity unless there is associated blockage, although commissioning criteria vary.
Rhinitis and chronic rhinosinusitis are primarily diagnosed on the basis of symptoms of blockage, rhinorrhoea, hyposmia and/or allergic symptoms. Blockaged due to inflammatory disease is usually bilateral or alternating. Start all patients suspected of having an inflammatory or allergic nasal condition on a regular daily intranasal steroid spray (fluticasone or mometasone) for a three-month trial, before re-evaluating the need for referral. Antihistamines are only of significant adjunctive benefit if there are allergic symptoms.
Patients with a known history of chronic rhinosinusitis, who are still symptomatic despite good compliance with regular intranasal steroids, should be referred for consideration of endoscopic sinus surgery.
Current evidence and guidelines
Chronic rhinosinusitis: EPOS European Position Paper on Rhinosinusitis and Nasal Polyposis 2020
In patients with allergic rhinitis and asthma, consider referring to the Allergic Rhinitis and its Impact on Asthma (ARIA) Guidelines 2010
https://cks.nice.org.uk/topics/allergic-rhinitis/
Authors
Mr Elliot Heward, ENT Registrar, North West Deanery
Mr Thomas Jacques, Consultant Rhinologist/ENT Surgeon, St. George’s Hospital, London