Lump in Throat
Red Flags requiring urgent ENT review:
· Acute dysphagia (+ not able to take solids or liquids)
· History in keeping with foreign body
Assessment
History
Duration
Constant or Episodic
Association with swallowing
Ability to swallow (dysphagia)
Voice change
Throat clearing
Neck movement and lumps
Reflux history
Previous episodes
Recent treatment or operations
Smoking and alcohol history
History of anxiety
Nasal symptoms (nasal obstruction, rhinorrhoea)
Malignancy red flags (weight loss, referred ear pain, neck lumps, night sweats, haemoptysis, odynophagia-pain on swallowing)
Examination
Mouth: Oral hygiene, ulceration or masses
Neck: movement (inability to move neck is torticollis), lymphadenopathy or masses
Nasal: Anterior rhinoscopy – atopic mucosa or polyps (Chronic rhinosinusitis)
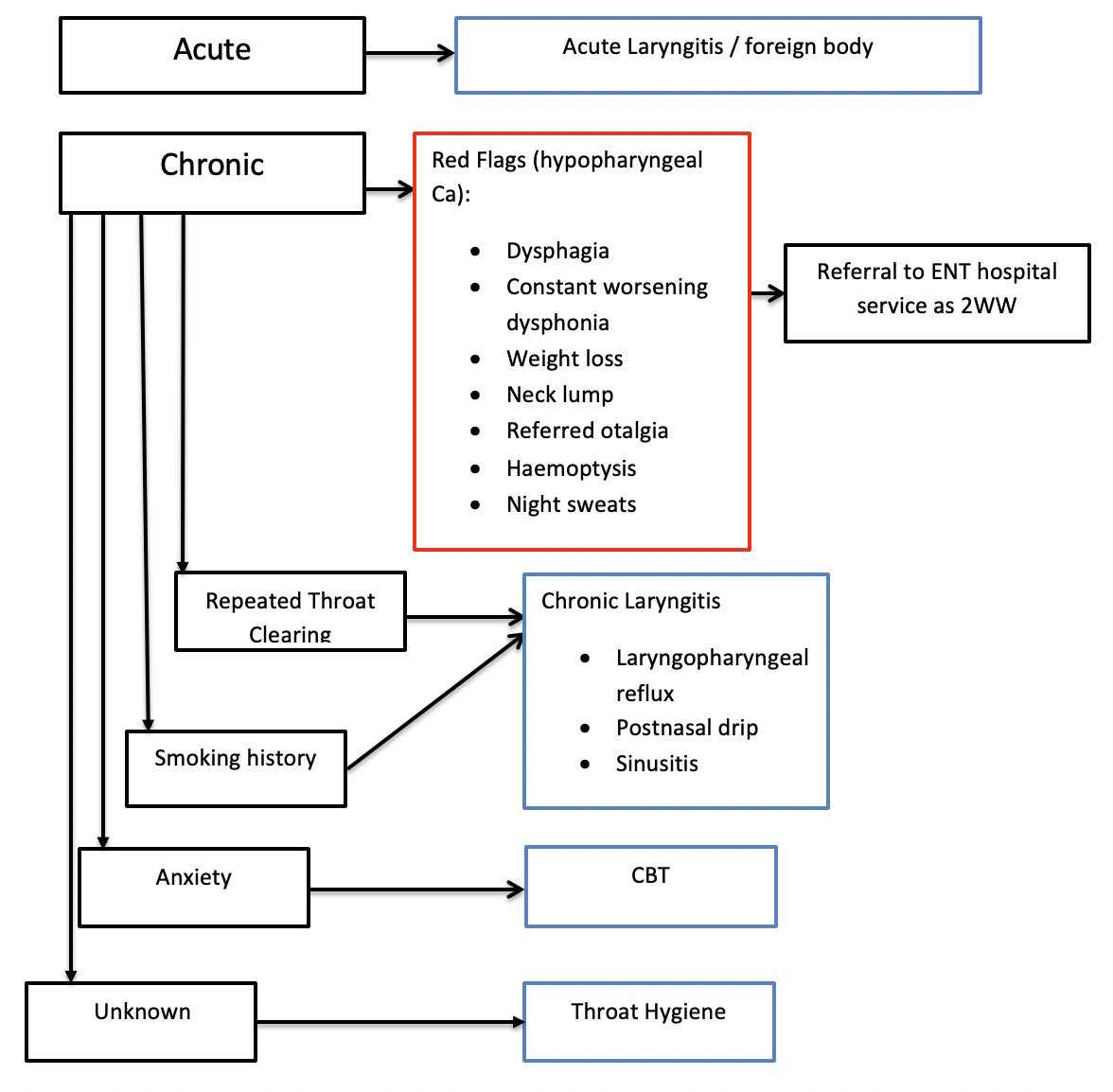
Differential Diagnosis
Globus pharyngeus (globus sensation)
It is the sensation of a non-painful lump in the throat. The aetiology is unknown. It is most commonly an intermittent sensation worse on swallowing. It is benign and difficult to manage. The majority of patients receive anti-reflux treatment as it can be difficult to differentiate between the conditions. Other causes include (upper oesophageal sphincter spams, oesophageal dysmotility, lingual tonsils and stress).
Laryngitis
Inflammation of the larynx can be caused by infection (URTI), irritation (laryngopharyngeal reflux or post nasal drip), allergy and overuse/trauma (profession voice use, coughing). Laryngitis can be acute or chronic (symptoms more than 3 weeks). Patients usually have hoarseness and pain in the throat. Acute laryngitis will self resolve with voice rest, avoidance of triggers and hydration. Treatment of the cause of chronic laryngitis is vital. All patients with non-resolving chronic laryngitis should be referred to ENT to rule out laryngeal pathology.
Foreign body
Acute onset where there is associated pain on swallowing (dysphagia) could indicate a foreign body. Following a meal would suggest a swallowed bone or sharp object which may be impacted into the throat or has traumatised the mucosa. These patients need to be referred to ENT on the same day for examination of the upper airway with a flexible nasoendoscope.
Laryngopharyngeal reflux
This is also known as silent reflux and is very common. Gastric contents (mainly activated pepsin enzyme) pass into the larynx or pharynx irritating the mucosal lining. Patients may complain of retrosternal burning or have risk factors for reflux (alcohol intake, weight, diet, eating late at night or spicy food). Patients can be given lifestyle advice (avoid alcohol, improve weight and diet, eat 3 hours before bed and avoid spicy food, exercise and sleep propped up) and a 3 month trial of a PPI and an alginate. These patients can be managed in primary care.
Chronic rhinosinusitis
Symptoms in keeping with chronic rhinosinusitis are nasal obstruction, rhinorrhoea, facial pain and change to smell in adults. Any patient with rhinorrhoea will likely suffer from post nasal drip where mucous passes through the post nasal space into the larynx. This can irritate the mucosal lining causing the need to throat clear and a sensation of a lump in the throat. Patients should be managed as per the EPOS guidelines most commonly with intranasal saline and corticosteroid sprays.
Anxiety
The link between anxiety and globus pharyngeus which is a sensation of a lump in the throat is well established. If physical causes have been excluded management of a patients anxiety with reassurance, medications, counselling or physiological therapy (eg. CBT) can be very helpful.
Laryngeal cancer
It is the second most frequent cause of head and neck cancer and 4 time more common in males. Smoking is the main risk factor. Patients who have chronic hoarseness with or without additional red flag symptoms such as: dysphagia, throat pain, neck lump, referred otalgia, haemoptysis or weight loss should be referred as a 2-week wait for review. NICE recommends all patients over 45 with persistent unexplained hoarseness to be referred as a 2 week wait. An urgent CXR is helpful to rule out chest pathology causing chronic hoarseness. Direct examination of the upper airway plus biopsy or imaging may be required.
Referral Pathways
Same day
Acute dysphagia (not able to take solids or liquids)
History in keeping with foreign body
Cancer-wait referral
Persistent symptoms of a lump in the throat with red flag symptoms
Routine referral
Patients with globus pharyngeus not responding to conservative management
More information
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4582871/
Author: Elliot Heward ENT Registrar North West Deanery