Sore throat
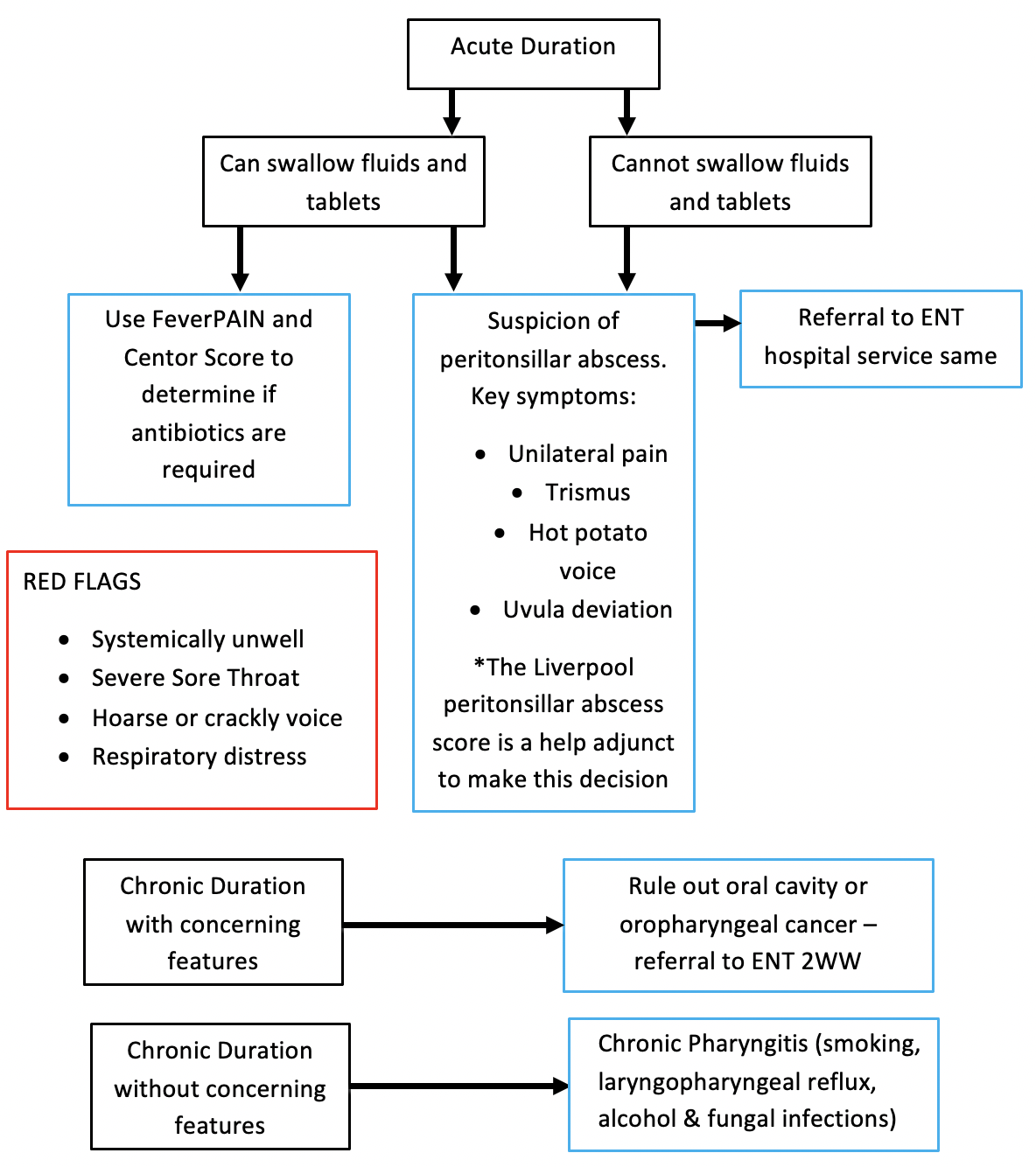
Flowchart
Red Flags requiring urgent ENT review:
Systemically unwell
Severe sore throat out of proportion to examination findings
Voice change
Respiratory distress
Assessment
History
Acute or chronic?
Bilateral or unilateral
Ability to swallow
Voice change
Referred ear pain
Neck movement and lumps
Previous episodes (No. of tonsillitis episodes)
Recent treatment
Malignancy red flags (dysphagia, weight loss, neck lumps, smoker)
Generalised fatigue (glandular fever)
Examination
Oropharynx: mouth opening (trismus implies peritonsillar/parapharyngeal abscess), uvula position (compare with central teeth), tonsil size/erythema/exudates, peritonsillar swelling , dentition
Neck: movement (neck stiffness concerning for deep neck space infection), lymphadenopathy or masses
Investigations
Do not perform a throat swab (SIGN)
Differential Diagnosis
Viral sore throat
The majority of sore throats are viral in aetiology and are difficult to differentiate from bacterial infections. Most infections are self limiting which last for around 1 week. The NICE and SIGN guidelines recommend using the Centor and FeverPain scoring to identify those who are more likely to benefit from antibiotics.
Tonsillitis
Patients with tonsillitis will usually have erythematous and swollen tonsils covered in exudate on examination. One tonsil can be more affected than the other, which can cause unilateral pain and an asymmetrical looking appearance. These cases are sometimes confused with a quinsy (see below).
Patients with recurrent tonsillitis should be referred to ENT for consideration for tonsillectomy if their frequency of symptoms meets the SIGN guidelines:
· 7 episodes in 1 year
· 5 episodes in both of the last 2 years
· 3 episodes in all of the last 3 years
Bleeding following a tonsillectomy is common. Rarely, it can be life threatening; therefore all patients with any severity of bleed should be referred to ENT via ED immediately.
For more information: https://entsho.com/tonsillitis
Peritonsillar abscess (quinsy)
Abscess between the tonsil and the pharyngeal muscle wall secondary to tonsillitis. Patients present with severe sore throat, hot-potato voice and trismus (reduced mouth opening). On examination the uvula will be deviated away from the affected side, and there will be a swelling superolateral to the tonsil, pushing it medially. Patients should be referred to ENT via ED for drainage, and can usually be discharged within 24 hours.
For more information, click here
Supraglottitis
This is similar to epiglottitis (although true epiglottitis in children is now rare). Patients present with a severe sore throat, hoarseness, dysphagia and drooling, and will develop stridor if untreated. Examination of the oropharynx will often be normal, therefore beware of patients with severe sore throat and normal tonsils, especially if hoarse. Refer patients to ED immediately.
For more info, click here
Liverpool Peritonsillar Abscess Tool: This is an excellent tool for helping to determine if a patient has a peritonsillar abscess objectively (see score below). A score ≥4 indicates a peritonsillar abscess.
Lau AS, Selwyn DM, Yang D, et al.The Liverpool Peritonsillar abscess Score: Development of a predictive score through a prospective multicentre observational study. Clin Otolaryngol. 2019;44:293–298. https://doi.org/10.1111/coa.13290
Link: https://onlinelibrary.wiley.com/doi/epdf/10.1111/coa.13290
Chronic sore throat
Chronic sore throat is a symptom of oropharyngeal, hypopharyngeal and laryngeal malignancy. Red flags to be aware of: dysphagia, odynophagia, referred unilateral ear pain, bleeding, neck mass, weight loss or difficulty opening the mouth. Squamous cell carcinoma is the most common malignancy of the upper aerodigestive tract. Lymphoma is the second most common type of tonsillar malignancy. Patients who are suspected to have oral cavity malignancy should be referred to ENT or Maxillofacial department depending on local availability.
Chronic pharyngitis is the most common cause of a chronic sore throat. Causes include laryngopharyngeal reflux, which is treated with lifestyle measures and alginates, smoking, alcohol, mouth breathing and fungal throat infections.
Referral Pathways
Same day
Suspicion of supraglottitis (999) or peritonsillar abscess
Tonsillitis associated with sepsis or inability to swallow liquids or medications
Cancer-wait referral
Chronic sore throat, especially with other red-flag symptoms
Routine referral
Recurrent acute tonsillitis meeting SIGN guidelines for tonsillectomy
More Information:
https://www.sign.ac.uk/assets/qrg117.pdf
https://www.nice.org.uk/guidance/ng84/chapter/Recommendations#managing-acute-sore-throat
Author:
Elliot Heward, ENT Registrar, North West Deanery
Mr Thomas Jacques, Consultant Rhinologist/ENT Surgeon, St. George’s Hospital, London