Stridor (children)
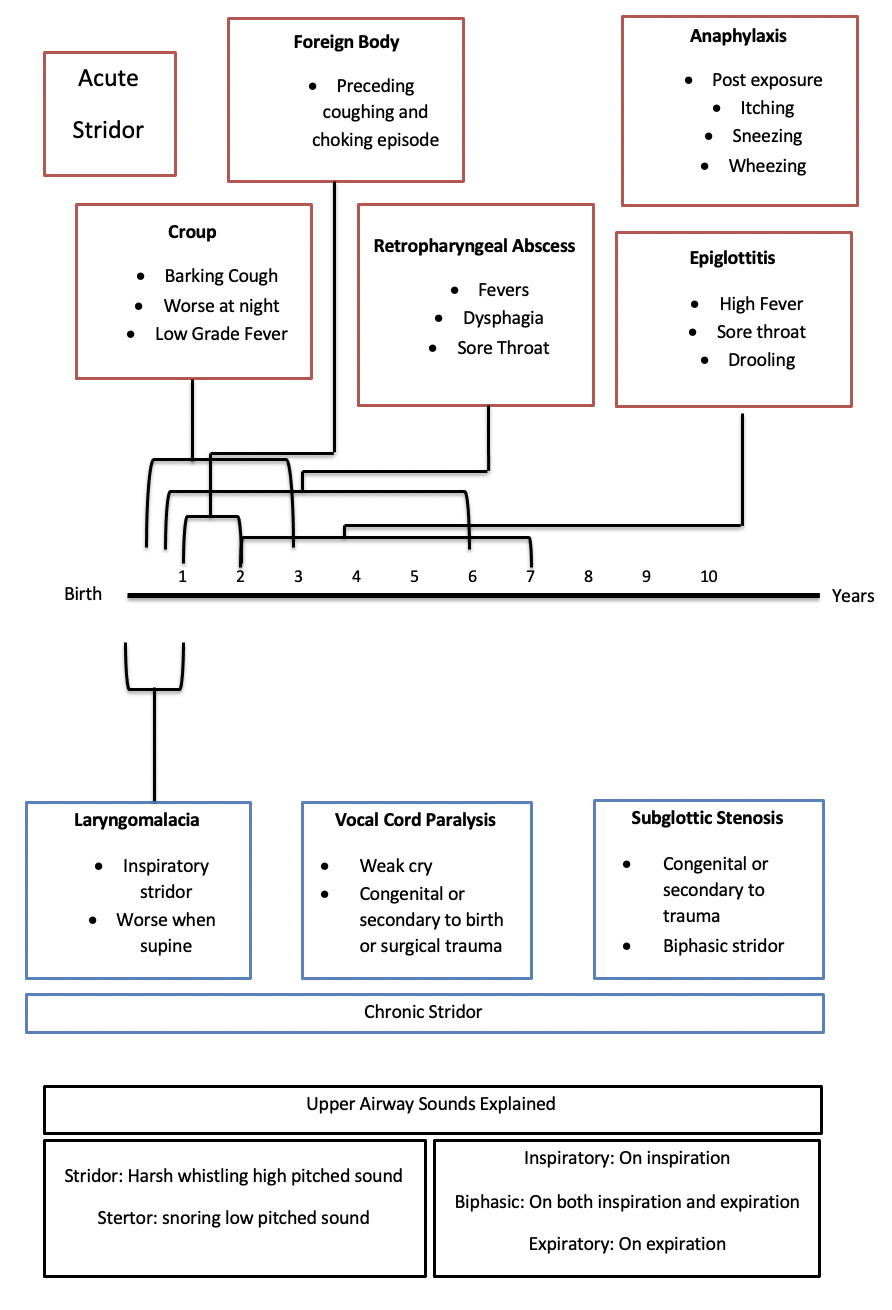
Differential Diagnosis
Red Flags requiring urgent ENT referral
All children with new onset stridor need urgent assessment in paediatric resus of A+E
Use judgement and assessment of respiratory status to determine urgency of referral.
Acute severe stridor, and any stridor with evidence of significantly raised respiratory effort should be considered emergencies.
Assessment
History
Duration
Constant or episodic
Improving or worsening
Triggers (Choking episode, Operations, Stay on PICU)
Association with feeding
Cry normal (if weak ?related to vocal cords)
Associated symptoms (sore throat, cough, dysphagia, itching, sneezing)
Birth history (trauma, PICU)
Family history
Development
Examination
Airway sounds - stridor (inspiratory, biphasic or expiratory) vs stertor (snoring sounds)
Respiratory effort (tracheal tug/recessions/cyanotic)
Oral examination: Trismus (not able to open mouth), Tonsil (erythematous, exudate), posterior pharyngeal wall (erythematous and bulging – retropharyngeal abscess)
Differential Diagnosis
Acute Stridor
Croup
Viral infection of the trachea and larynx causing inspiratory stridor, seal like barking cough and hoarseness. It is most common from 6 months to 3 years of age and occurs most commonly in the early winter. Parainfluenza is the most frequent viral pathogen. The majority recover in the community. Those who have respiratory distress or recurrent episodes need to be seen by the paediatric team. Very rarely do children need intubating. A child with frequently recurring croup may have an underlying upper airway condition (eg. laryngomalacia) which requires investigation by ENT.
Foreign body
Aspiration of foreign objects most commonly occurs in those under 3 years old. Small un-chewed objects can cause obstruction in the larynx, trachea or bronchial tree. Any child who has a choking or coughing episode regardless of their current state should be referred to hospital on the same day. Upper airway endoscopy may be required to rule out a foreign body.
Retropharyngeal abscess
This is a deep neck space infection that results from bacterial pharyngitis. Children will be systemically unwell with a fever and fatigue. They will commonly have a sore throat, dysphagia and trismus. Any child with these symptoms needs to be referred to ENT on the same day.
Epiglottitis
Presentation is similar to those with a retropharyngeal abscess (sore throat, drooling, fever). The most common age range is 2-7 years. Epiglottitis is becoming less common with the introduction of the Haemophilus Influenza B vaccination. Any child with these symptoms needs to be referred to ENT on the same day.
Anaphylaxis
Milk, eggs, wheat and soy are amongst the most common allergens for children. IgE mediated anaphylaxis causes itching, wheezing, facial and tongue swelling. Urgent intramuscular adrenaline is required and review on the same day in hospital to assess the airway.
Chronic stridor
Laryngomalacia
Abnormal development of the laryngeal cartilages (either or both the epiglottis or arytenoids) results in collapse of laryngeal structures which obstruct the airway during inspiration. Signs occur around 4 weeks of age, are worst at 6 months and resolve around 2 years of age. Babies have inspiratory stridor which is worse when supine and during sleep. Many babies also have reflux. Referral to paediatric ENT is required for direct visualisation of the larynx with a flexible scope. The majority require no surgical intervention.
Vocal cord paralysis
Children with vocal cord palsy present with biphasic stridor, weak cry aspiration and feeding difficulties. Causes include: congenital paralysis, birth trauma and iatrogenic (operations). There is an equal incidence of children with bilateral and unilateral vocal cord palsy. Children with airway compromise need immediate referral to a paediatric ENT centre.
Subglottic stenosis
This occurs below the vocal cords. It is caused congenitally or from intubation trauma which is why it’s important to know if the child has had any operations or been on PICU. It will present as a biphasic stridor. Children who present with recurrent croup may have an underlying subglottic stenosis which when inflamed causes airway obstruction. Patients need to be referred on the same day if in respiratory distress or routinely if has recurrent croup.
Subglottic haemangioma
These are cherry red swellings that can present within the larynx and cause stridor. Patients may also have a haemangioma in external parts of the body hence a complete examination of their skin and body is essential. These require assessment and management jointly by paediatrics and ENT. They can be treated conservatively, medically (with propanolol) or surgically.
Referral Pathways
Same day
Children with difficulty breathing
Children with signs suggestive of epiglottitis or retropharyngeal abscess
Suspected foreign body aspiration
Routine referral
Recurrent croup
Most causes of chronic stridor
More information
Author: Elliot Heward, ENT Registrar, North West Deanery